I’m not a fan of the “Kegel” as an all-purpose exercise to help strengthen the pelvic floor. Don’t get me wrong, I am grateful for the work of Dr. Kegel, an American gynaecologist who in the 1940s and 50s took an interest in women’s health and demonstrated how pelvic floor exercises could be used to improve symptoms of incontinence for women after childbirth, introducing a non-surgical option for treatment. He was a pioneer and an advocate for women’s pelvic health and well ahead of his time. (Note, while this blog post will refer in some places to women’s pelvic health, the concepts around the pelvic floor and kegels are applicable to men and those not identifying with the male/female binary – everyone has pelvic floor muscles and anyone can experience pelvic floor dysfunction).
Yet today there are several problems with the recommendation to “just do your kegels.”
First of all, unlike Dr. Kegel – who invented a device that was able to get biofeedback on the strength of the pelvic floor muscles during voluntary contraction and took the time to instruct his patients on how to do these pelvic floor exercises – most doctors today are not able to take the time with their patients to ensure they are doing pelvic floor exercises correctly. In fact research has shown that the majority of women are NOT doing them correctly. Many women are squeezing the wrong muscles or muscle groups and in some cases even bearing down when the action should be one of drawing up. Considering that excess intra-abdominal pressure is one of the main causes for pelvic floor dysfunctions like pelvic organ prolapse, we certainly don’t want to be bearing down during an exercise designed to improve our pelvic floor health.
Secondly, it is my understanding that Dr. Kegel taught the importance of both the contraction and the relaxation of the pelvic floor muscles. As with any skeletal muscle, the group of muscles known as the pelvic floor should have the ability to contract and the ability to release. A toned muscle does not equal a strong muscle. Muscles can only generate force when they are at an optimal length to do so and if they are being held in a constant state of contraction all the time they have no ability to generate any more force. You can’t contract a muscle that is already contracted – think of contracting your bicep into a bicep curl and staying there and how the muscle can’t generate any more force again until you bring the arm out of the curl. The emphasis on relaxation has been dropped in many conversations about kegels today that only talk about pelvic floor toning exercises.
Additionally, the majority of instructions given (when instructions are given) about how to do pelvic floor exercises are inadequate at best, and often just plain incorrect. I have read oodles of poor instructions available through Dr. Google and I have heard oodles more poor instructions given by yoga teachers (even teachers that teach teachers – teachers I studied with in Prenatal Yoga), doctors, nurses and complementary health care practitioners. While there are plenty of us trying to offer better advice, I believe the majority of people are not receiving good instruction on how (and when) to do pelvic floor exercises. If not done properly or for the correct purpose, just “doing your kegels” could be causing you more harm than good.
But more important than forgetting the importance of relaxation, and not receiving adequate assessment and instruction, the kegel is just not a functional exercise. It is being recommended beyond its useful purpose. While it may be useful for some people in some circumstances and as prescribed by a Pelvic Health PT who has evaluated your pelvic floor health and believes it important for your treatment, it is not an exercise we should all be doing multiple times per day as some kind of daily pelvic floor health regime or as prevention for problems we don’t have. And that is what I see happening all of the time.
Pregnant women are being given the advice to do kegels as prevention for pelvic floor dysfunction that is common post-birth and without any assessment to determine if they are already high tone (remember highly toned pelvic floors are also weak muscles). And if any population should be focusing on relaxing their pelvic floors it is pregnant women (the baby needs to move through the pelvic floor to come into the world so we want those muscles to yield!). The advice is coming from everywhere and it is common to speak to women that are under the impression they should be doing their pelvic floor exercises regardless of whether they are experiencing any symptoms of dysfunction. No! Stop the madness!
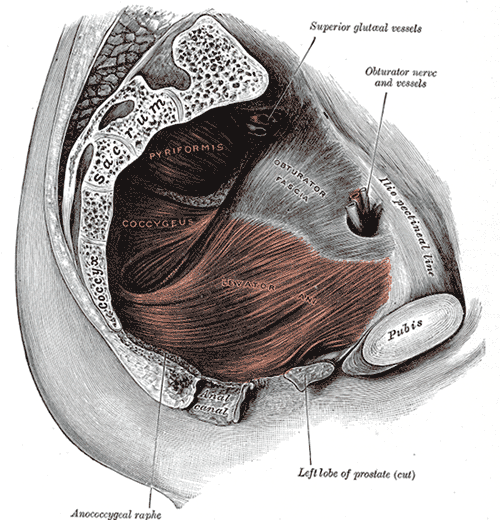
Your pelvic floor muscles do not exist in isolation from the rest of your body and the rest of your muscles. The pelvic floor is not one muscle but a group of muscles in layers. There are also muscles of the inner thigh, hip rotator muscles, gluteal (butt) muscles, abdominal muscles, and the diaphragm (your primary breathing muscle) that are intimately connected with the pelvic floor and pelvic floor health and function. To do isolated pelvic floor contractions as part of an everyday health regimen ignores the functional relationships this muscle group has with the rest of the body.
What we are really after with pelvic floor health is that we want our pelvic floor muscles to be able to respond appropriately (with the appropriate amount of force) to load. Jumping, sneezing, coughing and laughing all increase intra-abdominal pressure and therefore load. Pregnancy adds a load. We want a healthy and functional pelvic floor that can respond to changes in demand, changes to load. We want the pelvic floor to be able to continue to do its job in keeping things in, letting things out, providing support to help keep our pelvic organs in place, and teaming up with other muscle groups to stabilize our posture. And we want it to be able to do all these things while responding appropriately to load changes.
The pelvic floor muscles need to do their job all of the time, not just when we are thinking about them. Like the diaphragm, the primary breathing muscle, they’ve been working for us from the start without any special attention or workout regime. And that’s how it should be.
But there are some areas where we start to get into trouble and experience symptoms of pelvic floor dysfunction (pain, stress or urge incontinence, pelvic organ prolapse, etc.). And the problem with the universal kegel recommendation is that it assumes the pelvic floor muscles and their lack of strength are the root cause of any of these conditions AND because they might one day be the root cause of future symptoms we should keep exercising them to prevent dysfunction we don’t yet have.
Pelvic floor weakness can come from muscles that don’t have enough tone OR from muscles that have too much tone (think already in a kegel) OR even BOTH areas of low tone and areas of high tone. So if you are experiencing symptoms of pelvic floor dysfunction and you are high tone, doing kegels can make your condition worse, not better, if you are even able to do a kegel at all (you might be squeezing other muscles). But how do you know if you are high tone? If you are experiencing symptoms of pelvic floor dysfunction please get a referral to a Pelvic Health Physiotherapist so that you can get a proper assessment of whether you need to be focusing on relaxing the pelvic floor, strengthening it, or both.
But back to the pelvic floor not being the root cause……
Because the pelvic floor is in a relationship with the rest of your body (and your mind) there are many reasons why it might be experiencing low tone or high tone in the first place. And “doing your kegels” fails to address any of this.
Some of the major things that can affect pelvic floor health: poor sitting posture (sitting on your tailbone with the pelvis rocked back); heeled footwear (even small heels in running shoes or men’s shoes); stress, trauma, anger, and other emotions; events in childbirth; poor skeletal alignment (posture); poor breathing patterns; movement patterns; sitting too much & lack of movement/walking; muscle imbalances through the core causing the pelvic floor to over-compensate.
Here are some of the key areas I work with as a Yoga Therapist and Movement Educator when it comes to pelvic floor health:
- Look at how the breath pattern might be contributing to excess intra-abdominal pressure and work to re-establish a breathing relationship between the diaphragm and muscles of the pelvic floor and core.
- Look at how posture and movement patterns might be contributing to excess intra-abdominal pressure and work on strength and mobility exercises that give your body more freedom to choose different ways of moving. How your spine, pelvis and legs move together and independently is important.
- Using the breath and different awareness tools to begin to sense and establish a connection to the pelvic floor. You can’t tone or release a muscle you can’t even locate and differentiate from other muscles.
- Habit & lifestyle modifications: from how you sit to choices in footwear and clothing.
Where to begin? For some initial suggestions visit this older blog post. Then start to pay attention to your breathing and if you hold tension through your abdomen and pelvic floor. When you breathe in do your chest and shoulders rise upwards? Try to bring your awareness to your diaphragm, the breathing muscle that sits underneath your rib cage. On inhalation this muscle contracts and moves down (towards the pelvis). Can you let go of enough holding and tension through your core that you sense a response in the front, back, and sides of the torso as well as right down in the pelvic floor? Sense an expansion on inhale and a drawing back towards centre on exhale. Reflexively (i.e., you are not kegeling but allowing the movement to be in response to the breath and movement of the diaphragm). Can you allow this response to the diaphragm so that you no longer elevate your shoulders and collar bones when you inhale but instead sense the response of the whole system that is your core? Take your hands to your side ribs and keep your shoulders relaxed. Can you feel the expansion through your whole rib cage as well with the inhalation? Check in with this throughout the day. It should not feel like you are forcing the movement but that you are allowing your body to respond naturally to your breath.
Here is a video showing an exercise you can do every time you get in or out of a chair. It is a modified squat exercise that will tone your glutes/butt muscles eccentrically (without clenching them). Strong and functional glutes are important for walking well and in a way that also helps to eccentrically lengthen the pelvic floor muscles.
I hope this post has given you the confidence to stop “doing your kegels” (unless prescribed for you particular situation by a Pelvic Health PT) and has demonstrated that pelvic floor health, like the health of any body part, is dependent upon the larger connected Whole Body System.
I promise to write more blogs on the pelvic floor. Shorter ones. With more practice suggestions and videos. If you are interested to learn more, come to the Pelvic Floor Workshop on October 29 that I am co-teaching with Kaeleigh Brown, our local Pelvic Health PT. This workshop is open to people of any gender wanting to learn about their pelvic floor. If you are reading this after it has passed, we hope to offer it again. Keep an eye on upcoming Events.
The pelvic floor is a particular interest of mine and most of the yoga and movement classes and workshops I teach focus on breath awareness and movement that helps to uncover movement blind spots that often play a role in pelvic floor dysfunction. The pelvic floor is especially prominent in my Prenatal & Postnatal classes as well as my Pelvic Floor & Core Restore classes and I’m also available for private appointments. Feel free to contact me if you have any questions or comments. I’d love to hear from you!


